Autonomic neuropathy is a complex nerve disorder that affects the autonomic nervous system, which controls many of the body’s automatic and essential functions. These functions include heart rate, blood pressure, digestion, bladder control, sweating, and temperature regulation. When the nerves responsible for these processes are damaged, the body can struggle to maintain balance and stability.
Gaining clarity and understanding autonomic nerve damage is crucial for early recognition, proper treatment, and long term management. This blog explains what autonomic neuropathy is, what causes it, how it presents, and what treatment options are available for patients.
What Is Autonomic Neuropathy
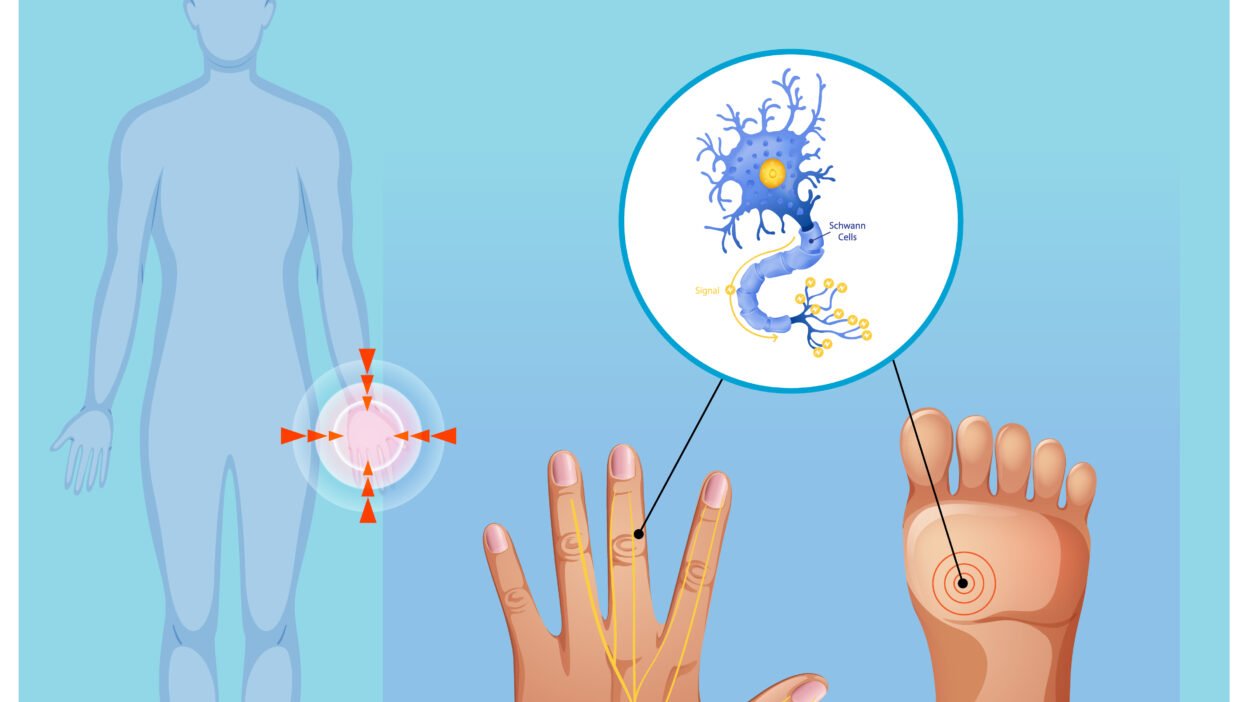
Autonomic neuropathy occurs when the nerves of the autonomic nervous system are damaged or impaired. Unlike sensory nerves, which allow you to feel pain or temperature, or motor nerves, which control movement, autonomic nerves work in the background without conscious effort.
These nerves regulate involuntary functions such as breathing rate, digestion, heart rhythm, blood pressure control, sexual response, and sweating. When they do not function properly, symptoms may affect multiple organ systems at once, making autonomic neuropathy difficult to recognize and diagnose.
The condition can develop slowly over time or appear more rapidly depending on the underlying cause. In some cases, symptoms may be mild at first but worsen if nerve damage continues.
Causes of Autonomic Neuropathy
Autonomic neuropathy does not have a single cause. Instead, it is often the result of another medical condition or long term nerve injury. Identifying the underlying cause is essential for selecting the most effective treatment approach.
Diabetes and Blood Sugar Disorders
Diabetes is the most common cause of autonomic neuropathy. Prolonged high blood sugar damages small blood vessels that supply nerves with oxygen and nutrients. Over time, this damage leads to nerve dysfunction. Poor glucose control increases both the risk and severity of symptoms.
Autoimmune and Inflammatory Conditions
Autoimmune disorders occur when the immune system mistakenly attacks healthy tissue, including nerves. Conditions such as lupus, Sjögren’s syndrome, and rheumatoid arthritis may cause inflammation that damages autonomic nerve fibers.
Neurological and Degenerative Diseases
Certain neurological conditions can affect autonomic nerve function. These include Parkinson’s disease, multiple system atrophy, and some forms of dementia. In these cases, nerve damage may worsen gradually as the disease progresses.
Infections
Some viral and bacterial infections can damage nerves either directly or through immune mediated responses. Examples include HIV, Lyme disease, and shingles. In certain cases, nerve symptoms may continue even after the infection has resolved.
Genetic and Hereditary Disorders
Some people inherit conditions that predispose them to autonomic nerve damage. These genetic disorders may cause symptoms earlier in life and often require specialized care.
Medications and Toxins
Exposure to certain medications, chemotherapy drugs, heavy metals, or excessive alcohol use can damage autonomic nerves. Reducing exposure and adjusting medications may help prevent further damage.
Also Read: https://sumssolution.com/
Common Symptoms of Autonomic Neuropathy
Autonomic neuropathy can affect many parts of the body. Symptoms vary depending on which nerves are involved and how severely they are damaged.
Cardiovascular Symptoms
The autonomic nervous system regulates heart rate and blood pressure. Damage can lead to:
- Dizziness or lightheadedness when standing
- Rapid or irregular heart rate
- Exercise intolerance
- Sudden drops in blood pressure
These symptoms increase the risk of falls and cardiovascular complications.
Digestive System Symptoms
Digestive function relies heavily on autonomic nerve signals. When these are disrupted, patients may experience:
- Nausea and vomiting
- Bloating or early fullness
- Constipation or diarrhea
- Delayed stomach emptying
Digestive symptoms can also interfere with proper nutrition and medication absorption.
Bladder and Urinary Symptoms
Autonomic nerve damage may affect bladder control and sensation. Common symptoms include:
- Difficulty emptying the bladder
- Frequent urinary tract infections
- Urinary incontinence
- Reduced awareness of bladder fullness
These issues may worsen over time if left untreated.
Sexual Dysfunction
Both men and women can experience sexual difficulties due to autonomic neuropathy. Men may develop erectile dysfunction, while women may notice reduced lubrication or arousal. These symptoms can significantly impact emotional well being.
Sweating and Temperature Regulation Problems
The autonomic nervous system controls sweat glands and temperature balance. Damage may cause:
- Excessive sweating
- Reduced or absent sweating
- Heat intolerance
- Difficulty adapting to temperature changes
These symptoms can make daily activities uncomfortable or unsafe.
Eye and Vision Changes
Autonomic neuropathy can affect how the pupils respond to light. This may lead to:
- Difficulty seeing in low light
- Sensitivity to bright light
- Slow adjustment when moving between light and dark environments
How Autonomic Neuropathy Is Diagnosed
Diagnosing autonomic neuropathy can be challenging because symptoms often overlap with other conditions. A thorough evaluation is necessary to confirm nerve involvement.
Medical History and Symptom Review
Doctors begin by reviewing symptoms, medical history, and any underlying conditions such as diabetes or autoimmune disease. Patterns of symptoms across multiple body systems often suggest autonomic nerve involvement.
Physical and Neurological Examination
A physical exam may include blood pressure and heart rate measurements in different positions, reflex testing, and evaluation of sweating and temperature response.
Autonomic Function Testing
Specialized tests help assess how well the autonomic nervous system is working. These may include:
- Heart rate variability testing
- Blood pressure response to posture changes
- Sweat testing
- Gastric emptying studies
- Bladder function assessments
Laboratory and Imaging Tests
Blood tests may identify diabetes, vitamin deficiencies, or autoimmune markers. Imaging studies such as MRI may be used to rule out other neurological conditions.
Treatment Options for Autonomic Neuropathy
Although autonomic neuropathy cannot always be reversed, many treatment options can help manage symptoms and slow progression. Treatment plans are typically individualized based on symptoms and underlying causes.
Treating the Underlying Condition
Managing the root cause is the most important step. This may include:
- Improving blood sugar control in diabetes
- Treating autoimmune inflammation
- Addressing vitamin deficiencies
- Adjusting medications that may affect nerve health
Controlling the underlying condition often prevents further nerve damage.
Medications for Symptom Management
Medications are commonly used to target specific symptoms, such as:
- Blood pressure medications for dizziness
- Drugs that improve stomach movement
- Medications for bladder dysfunction
- Treatments for erectile dysfunction
- Eye drops for dryness or light sensitivity
Symptom based treatment improves comfort and daily functioning.
Lifestyle and Supportive Therapies
Lifestyle changes play a key role in managing autonomic neuropathy. These include:
- Eating smaller, more frequent meals
- Staying hydrated
- Rising slowly from sitting or lying positions
- Wearing compression garments for blood pressure support
- Avoiding excessive heat
Physical therapy and gentle exercise can also help improve circulation and overall strength.
Mental and Emotional Support
Living with chronic nerve symptoms can be emotionally challenging. Counseling, stress management techniques, and support groups may help patients cope with the condition more effectively.
When to Seek Medical Care
Patients should seek medical attention if they experience unexplained dizziness, digestive problems, bladder issues, or changes in heart rate, especially if they have diabetes or another known risk factor. Early diagnosis allows for better symptom control and reduces the risk of complications.
Conclusion
Autonomic neuropathy is a serious condition that affects many essential bodily functions and can significantly impact quality of life. Early recognition, accurate diagnosis, and comprehensive treatment are key to managing symptoms and preventing further nerve damage.
By working closely with healthcare providers and staying informed about new developments, patients can take an active role in their care. Individuals interested in advancing medical understanding and future therapies may also explore distal sensory polyneuropathy study opportunities, which continue to expand knowledge and treatment options for nerve related disorders.